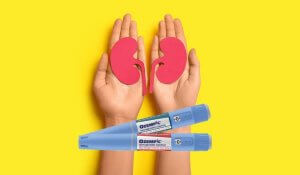
 In January 2025, the FDA approved Ozempic (semaglutide) to help treat patients with chronic kidney disease and diabetes. Semaglutide belongs to a group of drugs called glucagon-like peptide-1 receptor agonists (GLP1-RAs), which were originally approved to help control blood sugar in people with type 2 diabetes. Other forms of GLP1-RAs include Mounjaro, Wegovy, semaglutide, and tirzepatide. This new approval is an important step for people with both CKD and type 2 diabetes, as it provides a new way to manage these health issues.
In January 2025, the FDA approved Ozempic (semaglutide) to help treat patients with chronic kidney disease and diabetes. Semaglutide belongs to a group of drugs called glucagon-like peptide-1 receptor agonists (GLP1-RAs), which were originally approved to help control blood sugar in people with type 2 diabetes. Other forms of GLP1-RAs include Mounjaro, Wegovy, semaglutide, and tirzepatide. This new approval is an important step for people with both CKD and type 2 diabetes, as it provides a new way to manage these health issues.
What is a GLP1-RA and how does it work?
GLP1-RAs are a type of medicine that helps control blood sugar levels. They work like the natural glucagon-like peptide-1 hormone, which is released when a person eats. When blood sugar levels rise, this hormone triggers the pancreas to release more insulin, which helps move sugar from the blood into the body’s cells. At the same time, GLP1-RAs also stop the hormone glucagon from raising blood sugar levels. This combines to slow down digestion, keep blood sugar steady, and help people feel full for longer.
People with chronic kidney disease and diabetes can benefit from GLP1-RAs in several ways. These medications help protect the kidneys by lowering the chances of the disease getting worse or leading to kidney failure. GLP1-RAs also help control blood sugar levels, which reduces the amount of sugar reaching the kidneys and helps prevent damage to the kidney filters. GLP1-RAs can also help with weight loss, which is especially helpful for people with obesity and kidney problems. Losing weight can take some pressure off the kidneys and improve overall health.
Can a GLP-1RA replace other kidney medications?
 GLP1-RAs are not a replacement for other medications. Instead, they work alongside other treatments and are usually added to current plans to help control blood sugar and lower the chance of CKD getting worse. Besides the main GLP-1 RA medications mentioned above, there are some other common drugs that can be used to treat kidney disease and diabetes, or the conditions that can make CKD worse. These include:
GLP1-RAs are not a replacement for other medications. Instead, they work alongside other treatments and are usually added to current plans to help control blood sugar and lower the chance of CKD getting worse. Besides the main GLP-1 RA medications mentioned above, there are some other common drugs that can be used to treat kidney disease and diabetes, or the conditions that can make CKD worse. These include:
- Metformin and Kerendia, which help reduce blood sugar levels.
- SGLT2 inhibitors such as Jardiance, Invokana, Farxiga, and Stelgatro, which lower blood sugar and protect the heart and kidneys from further damage.
- ACE inhibitors such as Zestril and Vasotec, and ARBs such as Diovan HCT, Cozaar, Micardis, and Atacand, which are used to lower blood pressure.
Why should different kidney medications be taken together?
The development and progression of chronic kidney disease can happen for many reasons, and the underlying processes are complicated. Most treatments that focus on one specific cause of kidney damage tend to slow the disease only to a certain extent. Because of this, different treatments are needed to target multiple causes of kidney damage to help maintain kidney function.
For instance, treatments with blood-pressure controlling meds like ARBs and ACEs (grouped together as renin-angiotensin system blockers) and SGLT2 inhibitors can lower stress on the kidneys by reducing high filtration rates. On the other hand, non-steroidal mineralocorticoid receptor antagonists like Kerendia may help reduce inflammation and scarring in the kidneys, whereas GLP-1 receptor agonists work to address metabolic problems seen when kidney disease and diabetes co-incide. Each treatment works differently, and together they form a framework that can address various causes of CKD and improve patient outcomes.
The research behind using GLP-1 to boost health outcomes in kidney disease
The American Diabetes Standards of Care recommends combining SGLT2 inhibitors and GLP-1 receptor agonists for people with type 2 diabetes who have or are at high risk of heart disease. This approach may help lower the chances of heart and kidney problems.
The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines advise adding a medication mineralocorticoid receptor antagonist for patients who still have protein in their urine despite being on blood pressure medications and SGLT2i. KDIGO also recommends using GLP-1 as the preferred medication to lower blood sugar for these patients, as it can reduce the risk of heart-related events. Overall, these guidelines highlight the role of combining therapies like SGLT2i, GLP-1, and ns-MRA when treating patients. 
What about non-diabetic CKD?
Semaglutide in its injectable form is only approved for people with type 2 diabetes who also have chronic kidney disease (CKD). While most research supports using multiple treatments together for diabetes and kidney disease, there is less research available for kidney disease not related to diabetes.
Research is gradually showing more support for the potential of these medications in treating non-diabetic CKD. In the SELECT trial, data from over 17,000 people with obesity and heart disease but no diabetes showed that semaglutide reduced signs of kidney damage and slowed kidney decline. A smaller trial of around 100 people with obesity or overweight and CKD further showed that semaglutide lowered albuminuria, a marker of kidney damage, by about 50%.
For people with non-diabetic CKD, some options are now available, like Samsca for polycystic kidney disease. In addition, many treatments for glomerular diseases, especially IgA nephropathy, are being tested in advanced clinical trials.
These new treatments are good news for patients, doctors, and healthcare systems, but challenges do remain, such as deciding on treatment protocols and dosages.
FAQs
What does GLP-1 do to the kidneys?
GLP-1 RAs help protect the kidneys by slowing down damage. They work by lowering blood sugar levels, which prevents high sugar levels from harming the filters in the kidneys. They also reduce the amount of protein lost in urine, which is an early sign of kidney problems.
Which GLP-1 RA is best for patients with kidney disease and diabetes?
To date, the FDA has only approved Ozempic as a GLP-1 medication that helps lower the risk of kidney problems and heart-related death in adults with chronic kidney disease and diabetes.
Does GLP-1 RA reduce proteinuria?
GLP-1 receptor agonists can help reduce the amount of protein in urine, which is a sign of kidney damage. Less protein in urine means less strain on the kidneys, helping protect their function.
Is semaglutide safe for a non diabetic?
Semaglutide is usually safe for people without diabetes, but you should talk to a doctor first. Studies like OASIS 1 show that most people handle the medication well. However, it’s important to get checked by a doctor to make sure it’s right for you.













